Tibialis Posterior Exercises⁚ A Comprehensive Guide
This guide provides a comprehensive overview of exercises to strengthen and stretch the tibialis posterior muscle and tendon. It includes various exercises‚ progressing from basic to advanced levels‚ suitable for rehabilitation and prevention of tibialis posterior tendonitis. The exercises aim to improve flexibility‚ strength‚ balance‚ and overall foot function.
Understanding Tibialis Posterior Tendonitis
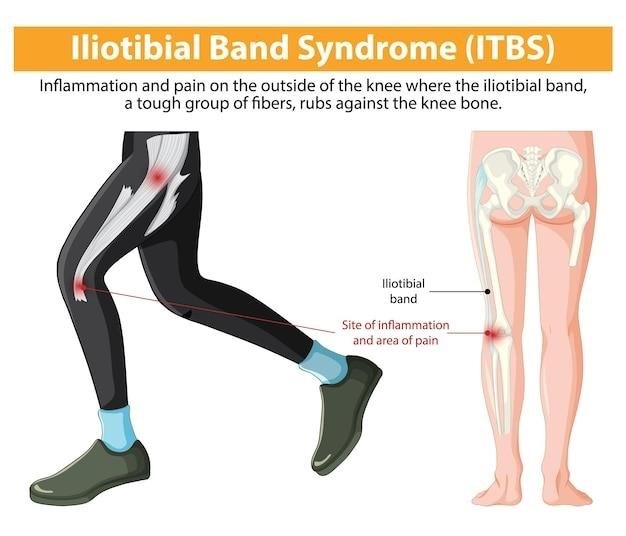
Tibialis posterior tendonitis‚ also known as posterior tibial tendon dysfunction (PTTD)‚ is a common condition affecting the tendon that runs along the inside of your lower leg‚ supporting your arch. This tendon plays a crucial role in ankle stability and foot movement. Inflammation of this tendon leads to pain‚ often accompanied by swelling and tenderness along the inner ankle and arch. Overuse‚ improper footwear‚ flat feet (pes planus)‚ and high impact activities can contribute to its development. The condition can range in severity‚ from mild discomfort to significant pain impacting daily activities. Early diagnosis and intervention are essential to prevent long-term complications such as flat foot deformity. Ignoring the symptoms can lead to chronic pain and functional limitations. Understanding the causes and recognizing the symptoms are crucial first steps in managing and treating tibialis posterior tendonitis effectively.
Causes and Symptoms of Tibialis Posterior Dysfunction
Posterior tibial tendon dysfunction (PTTD) arises from various factors‚ often involving a combination of overuse and underlying conditions. Overpronation‚ where the foot rolls inward excessively during weight-bearing‚ places significant stress on the tibialis posterior tendon‚ leading to inflammation and eventual dysfunction. High-impact activities like running and jumping can exacerbate this stress. Other contributing factors include obesity‚ which increases stress on the feet and ankles‚ and pre-existing foot conditions such as flat feet. Certain medical conditions can also increase susceptibility to PTTD. Symptoms of PTTD can vary but commonly include pain along the inner ankle and arch‚ often worsening with activity. Swelling and stiffness in the affected area are also prevalent. As the condition progresses‚ the arch may flatten‚ causing pain in the foot and ankle. In severe cases‚ the foot may become unstable‚ affecting gait and balance. Early diagnosis and appropriate management are crucial to prevent further complications and improve functional outcomes.
Initial Treatment⁚ RICE Protocol and Supportive Footwear
The initial management of tibialis posterior tendon dysfunction (PTTD) typically involves conservative measures aimed at reducing inflammation and pain. The RICE protocol—Rest‚ Ice‚ Compression‚ and Elevation—forms the cornerstone of this initial treatment phase. Resting the affected foot and ankle is crucial to allow the tendon to heal. Applying ice packs for 15-20 minutes at a time‚ several times a day‚ helps reduce inflammation and pain. Compression bandages can help minimize swelling and provide support to the injured area. Elevating the foot above the heart reduces swelling by promoting fluid drainage; In addition to the RICE protocol‚ appropriate footwear plays a vital role in supporting the foot and ankle and reducing stress on the tibialis posterior tendon. Supportive shoes with good arch support and cushioning can help prevent excessive pronation and reduce pain. Custom-made orthotics can provide additional support and correct biomechanical imbalances. These conservative measures‚ when implemented diligently‚ can significantly alleviate symptoms and facilitate the healing process‚ often paving the way for subsequent exercise interventions.
Exercise Progression⁚ From Basic to Advanced
A structured exercise program for tibialis posterior tendonitis should follow a progressive approach‚ starting with simple exercises and gradually increasing intensity and complexity as the condition improves. Initial exercises should focus on pain-free range of motion and gentle stretching. These might include ankle pumps‚ alphabet tracing with the foot‚ and towel stretches to improve flexibility. As pain subsides‚ strengthening exercises can be introduced‚ such as seated heel raises‚ which gradually progress to standing heel raises with resistance bands. Balance exercises‚ like single-leg stances‚ enhance proprioception and stability‚ crucial for reducing the risk of re-injury. Advanced exercises may incorporate plyometrics‚ such as jump squats and lateral hops‚ to improve power and agility. Throughout the progression‚ it’s vital to listen to your body and avoid pushing through pain. Regular self-assessment and monitoring of symptoms are crucial to ensure the exercises remain within tolerable limits. Modifying the intensity and duration of exercises based on individual responses prevents setbacks and promotes effective rehabilitation.
Strengthening Exercises⁚ Heel Raises and Resistance Band Work
Heel raises are fundamental for strengthening the tibialis posterior. Begin by performing seated heel raises‚ focusing on slow‚ controlled movements. As strength increases‚ progress to standing heel raises‚ initially holding onto a stable surface for balance. To increase resistance‚ utilize resistance bands. Wrap the band around your feet‚ maintaining tension while performing heel raises. This adds an extra challenge‚ further strengthening the tibialis posterior. Variations include single-leg heel raises‚ which target the muscle more intensely and improve balance. Ensure proper form throughout the exercises to avoid strain on other muscles. Start with lower repetitions and gradually increase the number as tolerated. Listen to your body; any pain should signal a need to reduce the intensity or take a break. Consistency is key; performing these exercises regularly is crucial for building strength and improving the condition of the tibialis posterior tendon. Remember to consult with a physical therapist for personalized guidance and modifications.
Stretching Exercises⁚ Towel Stretches and Wall Stretches
Towel stretches effectively target the tibialis posterior and surrounding muscles. Sit with your legs extended‚ looping a towel around the ball of your foot. Gently pull the towel‚ feeling a stretch in your calf and inner ankle. Hold this position for 15-30 seconds‚ repeating several times. For a variation‚ perform this stretch with your knee bent‚ targeting different muscle fibers. Wall stretches provide another effective method. Stand facing a wall‚ placing your affected foot behind you‚ heel on the ground. Lean forward‚ gently pushing your heel into the floor‚ feeling a stretch along the inner leg. Hold this stretch for 15-30 seconds‚ repeating as needed. Remember to maintain a straight back and avoid overstretching. These stretches improve flexibility and range of motion‚ which are crucial for alleviating tightness and preventing further injury. Proper stretching helps maintain the health and function of the tibialis posterior tendon‚ aiding in recovery from injury or preventing future issues. Always listen to your body and cease the stretch if you feel sharp pain.
Balance Exercises⁚ Improving Stability and Proprioception
Improving balance is essential for tibialis posterior rehabilitation‚ as this muscle plays a crucial role in ankle stability. Begin with single-leg stances‚ holding onto a chair or wall for support if needed. Gradually increase the duration of each stance as balance improves. Progress to more challenging exercises like standing on a foam pad or pillow‚ which further enhances proprioception (the body’s awareness of its position in space). These unstable surfaces require greater muscle activation to maintain balance‚ strengthening the tibialis posterior and surrounding muscles. Incorporate eye-closure during single-leg stances to increase the challenge and further enhance proprioception. Another effective exercise involves standing on one leg and performing slow‚ controlled ankle movements—circles or figure-eights—to improve both balance and range of motion. These exercises not only strengthen the tibialis posterior but also improve overall lower limb stability‚ which is crucial for preventing future injuries. Always maintain proper posture and avoid any movements that cause pain. As balance improves‚ gradually reduce the support and increase the duration or complexity of the exercise.

Advanced Exercises⁚ Plyometrics and Functional Movements
Once a solid base of strength and stability has been established through the basic and intermediate exercises‚ you can progress to more advanced exercises. Plyometrics‚ which involve explosive movements‚ are excellent for enhancing power and reactivity in the tibialis posterior; Begin with simple exercises like single-leg hops‚ progressing to more challenging variations such as lateral hops or jump squats. Always ensure proper landing technique to minimize stress on the ankle joint. Functional movements simulate real-life activities‚ further enhancing the practical application of the strengthened tibialis posterior. These exercises can include activities like walking lunges‚ side shuffles‚ or even jogging‚ but start slowly and gradually increase intensity. Incorporate changes in direction and terrain to enhance the challenge. Remember to listen to your body and stop if you experience any pain. As you progress‚ you can incorporate weights or resistance bands to increase the intensity of these movements. The goal is to gradually increase the load and demand on the tibialis posterior‚ leading to improved function and performance in daily activities and athletic endeavors. These exercises should be incorporated only after mastering the earlier stages of rehabilitation.
Preventing Recurrence⁚ Maintaining Strength and Flexibility
Preventing recurrence of tibialis posterior issues hinges on consistent maintenance of strength and flexibility. Continue performing the strengthening and stretching exercises regularly‚ even after symptoms subside. Aim for at least 2-3 sessions per week‚ incorporating both strengthening and flexibility exercises. Maintaining a balanced exercise program is vital‚ and incorporating activities that don’t overly stress the tibialis posterior is crucial. While running may be a favorite for some‚ consider incorporating low-impact exercises like swimming or cycling to maintain fitness without excessive strain on the ankle. Proper footwear plays a significant role in preventing re-injury. Ensure your shoes offer adequate support and cushioning‚ particularly in the arch area. Orthotics‚ if recommended by a healthcare professional‚ should be consistently worn. Regular self-assessment is key; pay close attention to any early signs of discomfort or weakness. Don’t hesitate to adjust your exercise routine or seek professional guidance if you notice any changes. Proactive management and consistent effort in maintaining strength and flexibility are essential to long-term prevention of tibialis posterior problems.
Importance of Professional Guidance⁚ Physical Therapy and Assessment
Seeking professional guidance is paramount in managing tibialis posterior issues. A thorough assessment by a physical therapist or other qualified healthcare professional is crucial for accurate diagnosis and personalized treatment planning. They can identify the underlying cause of your symptoms‚ rule out other potential conditions‚ and create a tailored exercise program suited to your specific needs and limitations. A physical therapist will guide you through proper exercise techniques‚ ensuring you perform them correctly to maximize effectiveness and minimize the risk of further injury. They can also monitor your progress‚ making adjustments to your program as needed. Furthermore‚ they can provide valuable advice on footwear‚ orthotics‚ and other supportive measures. Don’t underestimate the benefit of professional input; it can significantly improve outcomes and reduce the risk of long-term complications. Early intervention is especially important‚ allowing for prompt treatment and preventing the condition from worsening. A physical therapist’s expertise ensures a safe and effective rehabilitation process‚ ultimately leading to a faster and more complete recovery.
Additional Resources⁚ PDFs and Online Guides
Numerous online resources and downloadable PDFs offer further information on tibialis posterior exercises and management. These resources often provide detailed instructions‚ visual aids‚ and progressions for various exercises‚ supplementing the information presented here. However‚ it’s crucial to remember that these resources should not replace professional medical advice. Always consult with a healthcare professional before starting any new exercise program‚ especially if you have pre-existing conditions or experience pain. While online guides and PDFs can be helpful supplementary materials‚ they should be used cautiously and in conjunction with professional guidance. Look for reputable sources‚ such as those from established medical institutions‚ physical therapy clinics‚ or registered healthcare professionals. Be wary of information from unqualified sources‚ as inaccurate or incomplete instructions could lead to injury. Remember that a personalized approach is key‚ and a professional assessment will ensure the selected exercises are appropriate for your individual needs and condition. Use these additional resources responsibly to enhance your understanding and support your rehabilitation journey under professional supervision.